Table of Content
Hospice care allows patients and families to decide to a large degree what level of care they want. You can choose to receive services from one hospice discipline or from all hospice disciplines, such as nursing, social work, chaplain, home health aide, volunteers, music therapy, and others. Your care team will be a caring, respectful, understanding partner in the hospice journey. They are there to help take care of your loved one, not to take over. They will look to you for guidance and at the same time have the answers you need.
Here are expert insights about when, and how, to transition to hospice care. There are no rules on how to die or how to witness a loved one’s last moments—or last months. Some family members may attend early or frequently in the process, then not be there for the death itself. Even while in this state, always act as if the dying person is aware of what’s going on, and can hear what you’re saying and feel you touching them.
End-of-life changes at the time of death
There will be strong painkillers included, the use of which your hospice nurse will walk you through. We will deliver any necessary medication in your hospice care plan. If your elderly loved one has fallen often during the past six months, pay attention. Even falls that don’t result in injury can trigger anxiety and stress that can make caring for the patient even more emotional for their family. But if someone you love is dying, hospice can help to ease their pain and improve the experience of this period of their life—for them, and possibly for you, too. Body transportation will be coordinated between the family and the funeral home, with VITAS serving as an aid in the smooth planning of this process.

We will educate and provide information on pain and symptom management throughout the end-of-life journey. “Almost anybody can call in a referral for hospice,” says Dr. Landsman. Patients, family members, caregivers, and doctors can all request an evaluation for hospice enrollment.
Related to Palliative Care
On the first day of service, or shortly thereafter, your hospice nurse will order what is needed for that patient’s care. It could be a hospital bed, a walker, or an ambulance ride for certain types of appointments. Because, in this case, it is hospice care that has been chosen, there will not typically be physical or other types of therapy.
Part of this process involves informing our families about what to expect. Seasons Hospice is an independent community health care provider, not a large for-profit organization. We would not be able to offer our hospice services if we did not have the support of passionate community members who understand the importance of cost-free hospice care. To simplify the hospice process for patients and families, we rely on the generosity of our donors. At the very end of life, your support team will answer questions, make extra visits if needed for symptom management, and provide information about what to expect in the way of behaviors. After the patient has died, a hospice nurse will come to make the pronouncement and will deal with the death certificate for the funeral home.
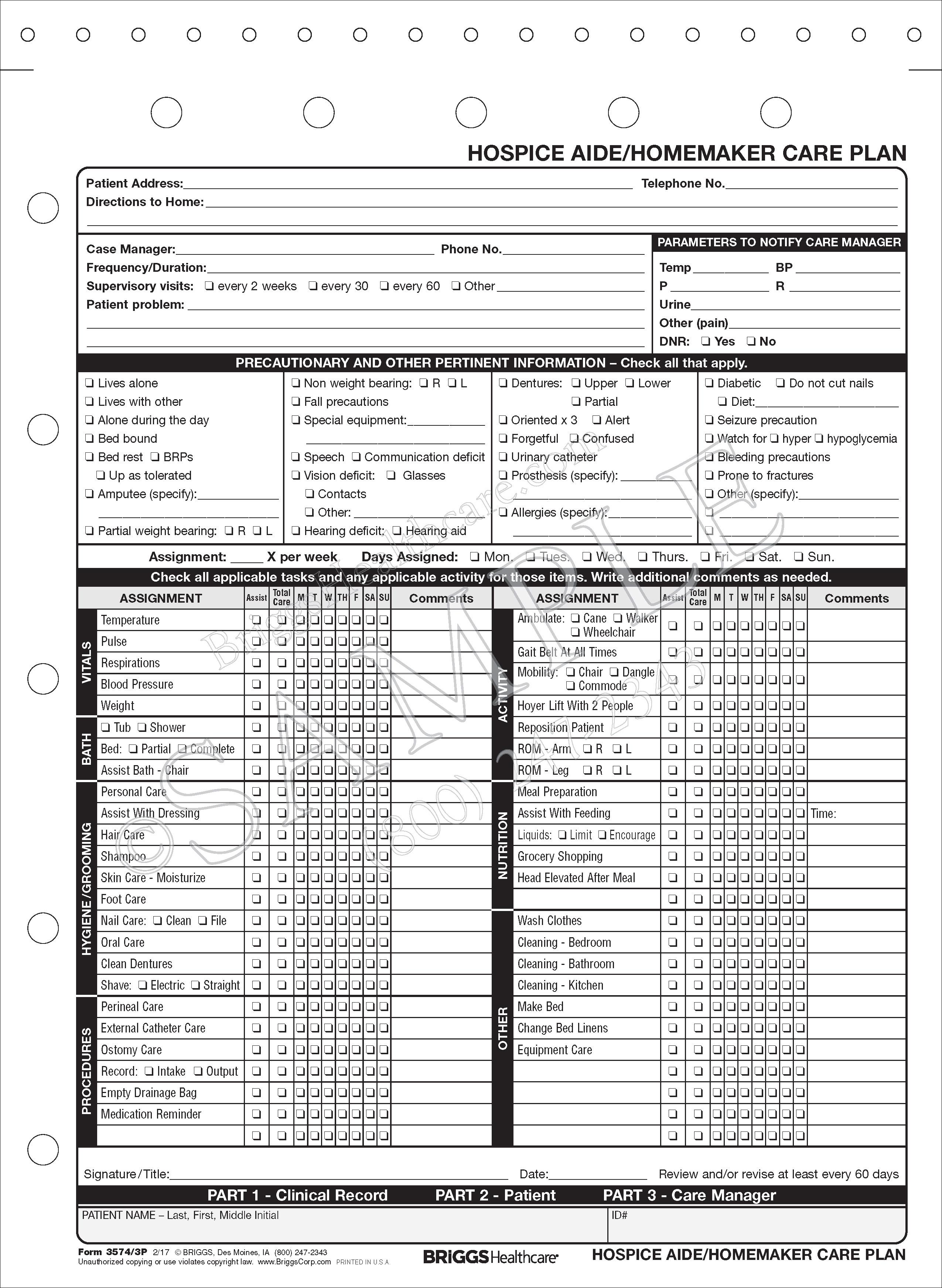
Your Hospice Care at Home Team Develops an Individualized Plan of Care
Throughout the patient’s end-of-life journey, the patient and family are the core of the hospice care team. Our highly skilled professionals work with you to understand the goals and needs, so we know the best approach to providing personalized care to your loved one. Your hospice care team will work with the patient and family to create a plan of care that provides comfort and accommodates the patient’s needs and goals. Once our initial plan is created, we continuously work with the patient and family to adjust based on the patient’s goals and condition.
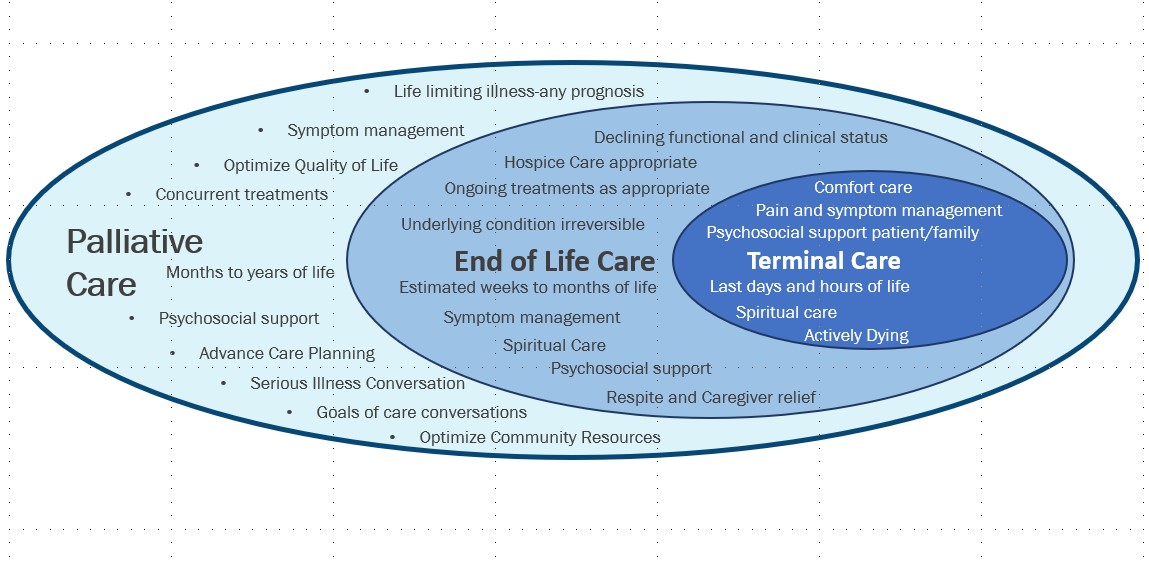
Samaritan is taking steps to protect patients, families, staff, and community from the Coronavirus. You may also get care at hospice centers, hospitals, nursing homes, and other long-term care places. Hospice differs from palliative care, which serves anyone who is seriously ill, not just those who are dying and no longer seeking a cure. When someone is terminally ill, family members and loved ones need to communicate with each other in order to make the best end-of-life care decisions. Tips for Visiting Someone on Hospice Hospice makes time for final words and second chances.
That plan is reviewed at weekly team meetings and revised based on the patient’s condition. The hospice team considers all input—from the patient, family, caregiver, physicians and the medical evaluation—to develop each patient’s plan of care. The plan is reviewed at weekly team meetings and revised based on the patient’s condition.

According to studies, hearing may be the last sense to leave a person who is actively dying. When breathing becomes irregular or seems difficult, with periods of no breathing lasting 20 to 30 seconds, the person may moan with each breath. This sound is typically caused by air passing over very relaxed vocal cords, and not due to pain or distress. The person may only need enough liquid to keep their mouth moist. It’s normal that as the person eats and drinks less, their output of fluids will also decrease.Read more about what hospice patients can eat and drink.
First of all, we have to certify that the patient meets the criteria for hospice care at home. They are normally bedbound, with a disease trajectory of six months or less, and they are seeking palliative care, not treatment for the disease. Family members should be discussing the prognosis and course of the illness, because the other most common feedback we receive is that they did not begin hospice care early enough. Because of advanced types of treatment, we see patients entering hospice care later and later.
Uncontrolled pain lowers the quality of life and may interfere with decision-making. That’s why palliative care works with patients from the very beginning to learn their wishes when it comes to pain management. When you or someone you love is diagnosed with a serious or advanced illness, life becomes overwhelming.
Lack of oxygen or organ shutdown can also cause extreme drowsiness. End-of-life changes in consciousness might be difficult to pinpoint if your loved one has been sick for a long time, especially with an illness related to their memory or cognition. However, any significant changes in a terminally ill person’s energy or wakefulness may warrant a call to the doctor. “The hospice team focuses on … managing symptoms at end of life, such as pain, shortness of breath, and decline in physical or cognitive functioning,” says Prescott. As a person’s body succumbs to disease, infections often occur more frequently. Pneumonia and urinary tract infections are especially common at the end, according to the National Institute on Aging.

Symptoms may include, but are not limited to, shortness of breath, fatigue, loss of appetite, difficulty sleeping, and nausea. The goal is to help people regain their strength so they can enjoy a better quality of life. Hospice care is person-centered care, meaning that it focuses on all aspects of the person’s well-being. Hospice care often focuses on maintaining the patient’s emotional and mental stability through a focus on their beliefs and wishes. Your hospice team will be extremely professional, not in a harsh or disconnected manner, but in a way that makes you feel safe and secure.
Compassion is essential not only for the patient but also for the patient’s family. Carers may be taught to be compassionate, but kindness and empathy are also a natural part of who they are. Your team will come up with a special plan just for you and your loved ones. They will check on you regularly, and a member of the team is on call 24 hours a day, 7 days a week. You might decide you or your loved one wishes to stay where friends and family can visit freely.